Procedures: Parathyroidectomy
Parathyroidectomy is the removal of one or more parathyroid glands. This page will focus on the procedure of parathyroidectomy.
What is a parathyroidectomy?
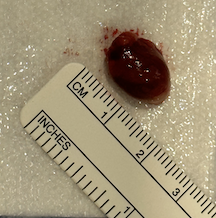
Enlarged parathyroid gland shortly after its removal.
A parathyroidectomy is a surgical procedure that involves the removal of one or more of the parathyroid glands. This is undertaken mostly for primary hyperparathyroidism, occasionally for tertiary hyperparathyroidism, and rarely for secondary hyperparathyroidism.
What are the surgical implications of anatomic variability in parathyroid glands?
Anatomic variability in parathyroid glands poses significant implications during surgical operations in the low central neck, particularly during procedures like thyroidectomy or parathyroidectomy.
Normal (orthotropic) location of four parathyroid glands.
Abnormal (ectopic) location of parathyroid glands. Source: The Parathyroid Gland: An Overall Review of the Hidden Organ for Radiologists - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Schematic-of-orthotopic-and-ectopic-parathyroid-glands-with-ectopic-parathyroid-adenomas_fig1_378304791 [accessed 25 Nov 2024]
Number of Glands: While most individuals have four parathyroid glands, some people have fewer while others have additional glands. The presence of accessory parathyroid glands can lead to persistent or recurrent hyperparathyroidism when the accessory gland(s) account for the hyperparathyroidism.
Location Variability: Parathyroid glands anatomic position is variable. While the anatomic position of parathyroid glands is often in a predictable area, behind the thyroid gland in the groove between the trachea and the esophagus, it is fairly common for them to be well outside of this region. These ectopic glands may be located high in the neck (having not descended during development), behind the esophagus, on the surface of the carotid artery, or even within the chest. This poses a significant challenge surgically.
Size and color: Normal parathyroid glands are small—about the size of two pieces of rice stuck together. Hyperactive glands are usually larger, and glands that are relatively inactive may be smaller. The color of parathyroids is similar to the color of lymph nodes and fat, especially when some blood is present in the surgical field.
Nerve Relationship: The parathyroid glands are usually closely associated with the recurrent laryngeal nerve. Anatomical variability may affect the nerve's course, which raises the potential for recurrent laryngeal nerve injury during surgery.
parathyroid autotransplantation
On occasion, when parathyroid tissue has been removed or has no remaining blood supply, it may be implanted (autotransplanted) into a muscle, where the rich muscular blood supply can allow the parathyroid tissue to live and function.
What are the risks of parathyroidectomy?
Parathyroidectomy carries certain risks for the patient to understand before electing to proceed with the procedure. These risks include:
Damage to Surrounding Tissues: With parathyroid gland surgery comes risk to nearby structures. This may include injury to the following structures:
thyroid gland
normal parathyroid gland(s)
nerves, such as the recurrent laryngeal nerve(s), the superior laryngeal nerve(s), the vagus nerve, the phrenic nerve, and other nerves
the esophagus
the trachea
blood vessels, including the internal jugular vein(s) and the carotid artery(-ies)
lymphatic structures, including the thoracic duct with a chyle leak
muscles involved in swallowing (such as the sternohyoid and sternothyroid muscles)
Persistent hyperparathyroidism: When one or more overactive parathyroid glands remain after parathyroid surgery, hyperparathyroidism may persist. This may require additional surgery.
Hypoparathyroidism: Removal of parathyroid glands can lead to low levels of parathyroid hormone, resulting in hypoparathyroidism and resulting low blood calcium. Consequences of low calcium can cause tingling, muscle cramps, or even an irregular hearth rhythm or seizures in severe cases. Permanent hypoparathyroidism is uncommon, and occurs when less than 1/2 of one normal parathyroid is functional. More commonly, hypoparathyroidism after parathyroid surgery is a temporary condition in which the normal parathyroid glands, which had atrophied due to lack of activity during the period in which one or more hyper functioning parathyroids had been driving blood calcium levels too high. After parathyroidectomy, these normal but essentially dormant parathyroid glands build activity and allow a return to normal parathyroid function.
Bleeding: As with any surgery, there is a risk of bleeding during or after the procedure. Bleeding in the low central neck may, in some cases, put pressure on the trachea (wind pipe) and affect breathing.
Infection: The surgical site may become infected, which could require additional treatment.
Anesthetic Risks: General anesthesia carries its own set of risks, including reactions to medications and breathing complications.
Other risks: It is impossible to list all potential problems after a surgical procedure.
How much surgical dissection is necessary in a parathyroidectomy?
The extent of surgical dissection required during a parathyroidectomy is contingent upon various factors, including the type of surgery being performed (open vs. minimally invasive), the anatomical variations of the parathyroid glands, and the presence of any associated pathologies, such as parathyroid adenomas or all-gland hyperplasia.
In a traditional open parathyroidectomy, a larger dissection may be necessary to fully visualize and confirm the location and number of affected glands. This approach typically involves a standard neck incision and exploration of the parathyroid glands, allowing for the identification and removal of abnormal tissues. The surgeon needs to carefully dissect through the surrounding tissues, which may include the thymus gland and surrounding fat, to gain optimal access to the parathyroid glands.
Conversely, minimally invasive techniques, such as focused parathyroidectomy, involve less dissection. These methods aim to limit the surgical field to the location of the targeted parathyroid gland, often utilizing less invasive access points, thereby minimizing trauma to surrounding tissues. This approach is most effective and applicable in cases where preoperative imaging has accurately localized the abnormal parathyroid gland.
Regardless of the technique employed, adequate dissection is part of ensuring complete removal of the hyperactive parathyroid tissue while preserving surrounding structures, notably the recurrent laryngeal nerve and nearby blood vessels. The surgical team must balance the need for sufficient exposure with the goal of minimizing complications and promoting quicker recovery.
What adjunctive information may used by a surgeon during parathyroidectomy?
During a parathyroidectomy, a surgeon may utilizes several adjunctive information sources to enhance the procedure's effectiveness and patient safety. These include the following, and items 1-3 are standard, but items 4-10 vary depending on the surgeon’s practice:
Patient History and Physical Examination: An understanding of the patient's medical history, current medications and symptoms is important.
Hormonal and Biochemical Analysis: Preoperative serum calcium, parathyroid hormone, kidney function and sometimes analysis of a 24 hour urine output is fundamental to the accurate diagnosis of hyperparathyroidism.
Knowledge of Anatomical Variations: The surgeon’s knowledge of normal anatomy as well as possible anatomical variations in the parathyroid glands is important.
Imaging Studies: Preoperative imaging, such as nuclear medicine imaging (Sestamibi or SPECT-CT), ultrasound, CT scans, or MRI, helps localize abnormal parathyroid glands. This information guides the surgeon to the specific anatomical location.
Nerve Monitoring: In some cases, intraoperative monitoring of the laryngeal nerves is employed to assist in the surgeon’s identification and preservation of the laryngeal nerves.
Float test: Parathyroid glands typically sink in water or saline, whereas fat and normal lymph nodes will float. Removed tissue may be tested in this way to assist in the surgeon’s assessment.
Intraoperative Parathyroid Hormone (PTH) Monitoring: Measuring PTH levels during surgery allows the surgeon to assess the removal of hyperfunctioning parathyroid tissue. A significant drop in PTH after excision is correlated with successful resection.
Frozen section analysis: During surgery, tissue may be sent to a pathologist to perform real-time microscopic examination of a tissue. For parathyroid surgery, this typically involves identification of whether the submitted tissue is in fact parathyroid tissue, and not a lymph node, thyroid tissue, or other tissue. Sometimes, the pathologist can identify an increased density of parathyroid cells that may support the diagnosis of a parathyroid adenoma.
Intraoperative Parathyroid Hormone (PTH) Monitoring: Measuring PTH levels during surgery allows the surgeon to assess the removal of hyperfunctioning parathyroid tissue. A significant drop in PTH after excision is correlated with successful resection.
Surgeons may use additional adjunctive technologies like radio guidance (pre-operative injection of a radioactive substance that preferentially concentrates in parathyroid glands and may be detected with. probe during surgery) or injection of methylene blue (which preferentially collects in parathyroid glands, assisting in visual identification.
Is parathyroidectomy ever repeated?
Revision parathyroidectomy refers to the surgical procedure aimed at correcting persistent or recurrent hyperparathyroidism after an initial unsuccessful surgery.
Reasons for needing a revision parathyroidectomy include missed hyperfunctioning parathyroid tissue during the initial operation, or the subsequent development of hyperfunctioning parathyroid tissue after an initial surgery.
The approach for revision surgery often involves imaging techniques such as ultrasound, sestamibi scans, or CT scans, which can help localize the parathyroid tissue that may not have been identified with the first procedure.
Recovery
Typical incision for parathyroidectomy. The redness fades after about 2 months.
Usually, a patient will stay in the hospital or surgery center overnight after parathyroidectomy and, if recovering normally, be discharged to home the following day. A normal diet is typically begun shortly after surgery. Pain is usually moderate, especially with swallowing, but quickly improves over a few days. Supplemental calcium or vitamin D along with additional outpatient blood tests may be used until normal calcium and parathyroid function is demonstrated.
This page