Procedures: Parathyroid Autotransplantation
What is parathyroid autotransplantation?
In a word, parathyroid gland tissue may be moved (transplanted) to a different part of a person’s own (auto) body.
Why is parathyroid autotransplantation performed?
There are two reasons parathyroid autotransplantation is undertaken:
During the course of surgery in the central neck, if a normal parathyroid gland has lost it’s blood supply, it may be autotransplanted in order to give it a chance of surviving, and continuing to function long-term.
In the case of hyperparathyroidism surgery, where all four parathyroid glands are overactive, removing all four glands and auto transplanting one half gland (a 3 1/2 gland parathyroidectomy) may be undertaken. This is done to treat the hyperparathyroidism, but also to try to avoid hypoparathyroidism.
How is a parathyroid autotransplantation performed (technically)?
Once a parathyroid has lost its blood supply, it begins to die. Parathyroid gland tissue may survive if it is placed into a bed of tissue with excellent blood supply. Muscle is an excellent choice of tissue to receive parathyroid tissue because muscle is readily available either in the neck or elsewhere, is not damaged by the process, and it has an excellent blood supply. If the gland can absorb enough oxygen through diffusion to survive in its new location, it can then grow new blood vessels and function normally. In order to maximize survival of transplanted parathyroid tissue, the parathyroid to be transplanted is typically cut into many tiny pieces before being placed in the muscle in order to maximize the surface area to volume ratio and hence the tissue’s ability to absorb oxygen by diffusion. The minced parathyroid is placed in one or more tiny pockets of muscle created by incision. The muscle pocket is then closed with a clip or a suture.
Where is a parathyroid autotransplanted?
During surgery for a condition other than four gland parathyroid hyperplasia, a parathyroid gland may be transplanted into a nearby convenient muscle, such as the sternocleidomastoid muscle, which is accessible through the incision already being used.
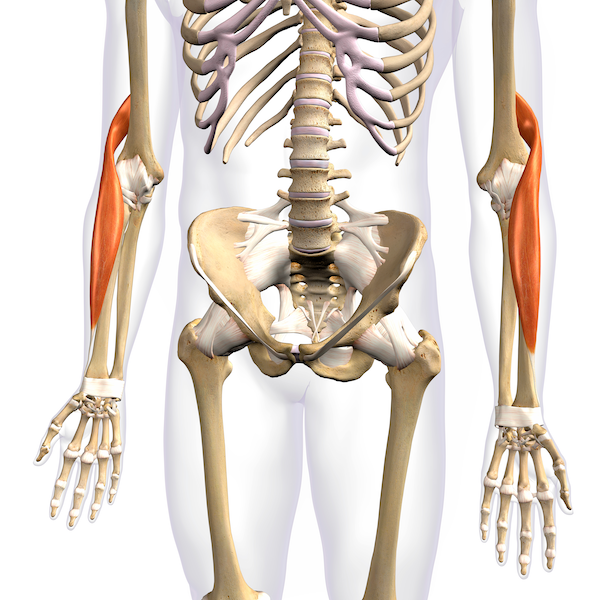
Brachioradialis muscles
The recipient site for parathyroid autotransplantation is often different when a procedure is being performed for four gland (all gland) parathyroid hyperplasia. When a 3 1/2 gland parathyroidectomy is being performed for four gland hyperplasia, all four glands are removed, but 1/2 of one gland is re-implanted in a muscle elsewhere The brachioradialis muscle of the forearm, just by the elbow, is often chosen as a recipient bed for safety reasons. Since the disease process leading to four gland hyperplasia is genetic and not reversed by surgery, the reimplanted 1/2 gland may eventually grow and produce too much parathyroid hormone. In this case, surgery to remove some of this implanted parathyroid gland is needed. Returning to the natural parathyoid position in the neck, near the laryngeal nerves in particular, would have higher risk than returning to the forearm. An additional reason to use the forearm as an implant site is that should primary hyperparathyroidism recur after 3 1/2 gland parathyroidectomy, it would be helpful to be sure that the excess parathyroid hormone is coming from the reimplanted 1/2 gland rather than a possible 5th parathyroid gland in the neck or chest, which is an anatomic variant occasionally present. To verify this, a blood draw for parathyroid hormone could be taken from the upper arm on the side of the implant and simultaneously from another area, such as the opposite arm. If the implanted parathyroid is truly the cause for recurrent parathyroid hormone, then the parathyroid hormone level in blood drawn from the implanted arm would be significantly higher than that from the other blood draw site.
How long does it take for autotransplanted parathyroid to begin functioning?
Up to a month or so. Blood testing for parathyroid hormone indicates if and when parathyroid tissue is producing parathyroid hormone.
Is parathyroid autotransplantation always successful?
Parathyroid autotransplantation has a reported success rate of 93%.
This page