Diagnostics: Needle Biopsy
A needle biopsy is a low-risk way to gain vitally important information about the nature of a mass (growth, lump, etc.). The concept is simple: remove a tiny sample of the abnormal tissue, place it on a glass slide, and a pathologist looks at it under a microscope to help determine what type of tissue it is and whether it appears to be cancer. If needed, additional genetic or molecular testing may be performed on a needle biopsy specimen to characterize it better.
Needle biopsies are often performed with the advantage of some sort of imaging technology, such as an ultrasound or CT scan, so that the needle may be guided into the target lesion precisely.
A fine needle aspiration biopsy (FNAB) is a technique in which a very small caliber (fine) needle is used to remove cells from a target, such as a thyroid nodule, an enlarged lymph node, or a mass of the parotid gland (using examples from the head and neck area). An advantage of this technique is that the needle is small but a disadvantage is that the cells removed are in tiny clusters that do not demonstrate the pattern of cell arrangement (the architecture) of the tissue well. Sometimes, genetic testing may be performed on a fine needle biopsy specimen, and genetic testing may prove helpful in some circumstances.
A core needle biopsy is a technique in which a larger caliber needle is used to obtain a solid piece of the target tissue. While still small in the grand scheme of things, the core biopsy material is large enough that the architecture of the tissue may be visible, and other testing such as performing special molecular stains (such as p16) or flow cytometry (to test for lymphoma) may be undertaken.
A core needle biopsy device has a larger needle size and a mechanism to facilitate obtaining the biopsy.
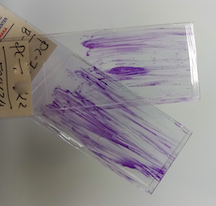
Microscopic view of a core needle biopsy specimen, which is large enough for cell arrangement to be preserved and interpreted by the pathologist, as well as for special testing such as molecular staining and flow cytometry.
This page