Treatments: Parathyroid
Outside of surgery or trauma, naturally occurring parathyroid disease is a mater of too much parathyroid hormone (hyperparathyroidism), which may be produced by one or more of the parathyroid glands. Surgery or trauma to the neck, especially total thyroidectomy and central neck lymph node removal are the usual causes of insufficient parathyroid hormone production (hypoparathyroidism), which may be temporary or permanent.
parathyroidectomy
Surgical removal of one or more parathyroid glands remains the mainstay for treatment of primary hyperparathyroidism as it renders a cure about 95% of cases. Surgery is indicated for selected cases of tertiary hyperparathyroidism, but rarely for secondary hyperparathyroidism when medications prove ineffective. Among cases of primary hyperparathyroidism, 85% are caused by a single overactive parathyroid gland, and its removal yields cure. Fortunately, due to two relatively recent advances (parathyroid imaging studies and intraoperative PTH measurements), parathyroidectomy may be performed in a minimally invasive approach with very high success rate. Pre-operative localization of the overactive parathyroid(s) may be done several ways, including use of a sestamibi or a SPECT scan.
What are the reasons/indications for undertaking parathyroidectomy?
Primary Hyperparathyroidism: This is the most common indication, where surgery is often recommended for patients with:
High serum calcium levels (>1 mg/dL above the normal range).
Symptoms of hypercalcemia (e.g., kidney stones, osteoporosis, fractures, fatigue, or gastrointestinal symptoms).
Bone disease associated with hyperparathyroidism.
The incidence of a single parathyroid adenoma is significantly more common in primary hyperparathyroidism compared to the rarer occurrences of double adenomas or four-gland hyperplasia.
Parathyroid Cancer: Parathyroid cancer is very rare, accounting for 1% of cases of primary hyperparathyroidism. Surgical intervention is required for the removal of malignant parathyroid tumors, primarily because of the risks associated with extreme elevation in blood calcium, but also because of the additional risks of cancer, such as invasion into normal structures, such as the recurrent laryngeal nerve, which controls the vocal cord.
Secondary Hyperparathyroidism: In cases where the hyperparathyroidism is caused by chronic kidney disease and results in severe symptoms that do not respond to medical management.
Tertiary Hyperparathyroidism: This occurs when parathyroid glands become autonomously functioning after long-standing secondary hyperparathyroidism after the kidney disease is cured (with a kidney transplant).
managing post-operative hypoparathyroidism (abnormally low parathyroid hormone levels)
As with muscles, unused parathyroids atrophy over time. When one parathyroid is over-active, thus raising the calcium level in the blood, the other parathyroid glands appropriately reduce their own production of parathyroid hormone. Once surgery is undertaken and the overactive gland has been removed, the other glands need some time to build up and produce the needed amount of parathyroid hormone. This is typically treated with oral calcium carbonate (such as Tums), but on occasion is treated with progressively more potent medications, such as vitamin D, calcium administer intravenously (while in the hospital), and even synthetic (recombinant) parathyroid hormone (Natpara). In cases of prolonged and presumed permanent parathyroid hormone insufficiency (after thyroidectomy or removal of lymph nodes in the area, for example), a long-term regimen of oral calcium, vitamin D, and if those are not effective, possibly recombinant parathyroid hormone (Natpara) is used. In the short term, low calcium can cause a tingling sensation, muscle spasms, seizures, or irregularities in the heart rhythm; long term low calcium can lead to weak bones.
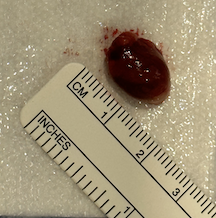
parathyroid autotransplantation into the forearm
On occasion, when all parathyroid glands are overactive, surgery is undertaken whereby all glands are removed, but one half of one gland is re-implanted into a muscle. Since a re-implanted parathyroid gland works just as well in the neck as anywhere else, reimplantation into a muscle of the forearm (the brachioradialis) is sometimes undertaken. This half of a gland may take up to a month to begin functioning again, but it usually does and with a much more normal state of blood parathyroid hormone levels. Implanting a half-gland in the arm is done to prepare for future contingencies. If the parathyroid hormone level in the blood is found to be high some time after the original parathyroid surgery, one would need to know if there is still hyperfunctioning parathyroid in the neck versus possible over-growth of the implanted half-gland in the arm. Two simultaneous blood draws from the left and right upper arm would indicate whether the overactivity is from the implanted arm or not. If the PTH level is significantly higher in the implanted arm than the other arm, then a relatively safer procedure may be performed to reduce the size of the implanted parathyroid gland may be undertaken. If, on the other hand, the parathyroid hormone level is equal in both arms, then chances are good that a retained parathyroid gland in the neck or chest exists, and a localizing study may be used to help locate it prior to surgery. from the l so that if, perhaps years after the original operation, the one-half gland that was implanted grows and becomes overactive, a safe and simple procedure removing some of this parathyroid gland from the arm may be done.
parathyroid autotransplantation into the neck
When surgery around the parathyroid glands is performed for reasons other than hyperparathyroidism, such as thyroid surgery, neck dissection, or laryngectomy, one or more parathyroid glands may be found to have lost their blood supply during the dissection. If there is no reason to believe a parathyroid in this situation is diseased, it may be reimplanted. In this case, since there is low risk of the parathyroid gland being overactive, it is typically implanted into a readily available neck muscle (such as the sternocleidomastoid muscle).
Medical treatment of hyperparathyroidism
If calcium and/or parathyroid levels are only mildly elevated, primary hyperparathyroidism may be treated non-surgically. Another reason for treating primary hyperparathyroidism medically is when the affected individual is not healthy enough to undergo even a relatively minor surgical procedure.
A group of drugs known as calcimimetics has been approved by the Food and Drug Administration for the treatment of secondary hyperparathyroidism (which is caused by kidney disease). These drugs work by stopping the production of PTH by the parathyroid glands. Although calcimimetics are intended for secondary hyperparathyroidism, some physicians prescribe them selectively for primary hyperparathyroidism.
Alternatively, possibly to put surgery off while one is healing from another medical problem, mild hyperparathyroidism could be managed with plenty of hydration, possibly a “water pill” (diuretic) that lowers blood calcium, and avoidance of drugs like lithium or thiazide diuretics that increase blood calcium. If this route is taken, then monitoring blood calcium levels (every 6 months), blood pressure (every 6 months), kidney function (every year), and bone density (every 1 to 3 years) is typically performed by the primary care physician.
This page