Conditions: laryngeal nerve dysfunction
(weakness, paralysis, and lack of sensation)
What are the laryngeal nerves?
The nerves that control movement of the vocal cords branch from the left and right vagus nerves, which originate from the brain. Most of the movement of the vocal cords comes from muscles controlled by the recurrent laryngeal nerves, which branch off of the vagus nerve in the chest, loop around an artery, and then travel back toward the vocal cords from below. On the way back up to the vocal cords, these recurrent laryngeal nerves run along the deep portion of the thyroid gland and the trachea (windpipe). A different nerve branch of the vagus nerve, called the superior laryngeal nerve, branches from a takeoff point higher in the neck. This superior laryngeal nerve has an external branch, which also crosses deep to the thyroid gland on its way to the cricothyroid muscle. The internal branch of the superior laryngeal nerve enters the larynx and serves to detect sensation on and around the surfaces of the vocal cords.
Surgical photo demonstrating the anatomy of the recurrent laryngeal nerve (“RL nerve”), the trachea, and the thyroid gland after it has been mobilized and lifted off of the trachea and nerve.
How do the vocal cords normally function?
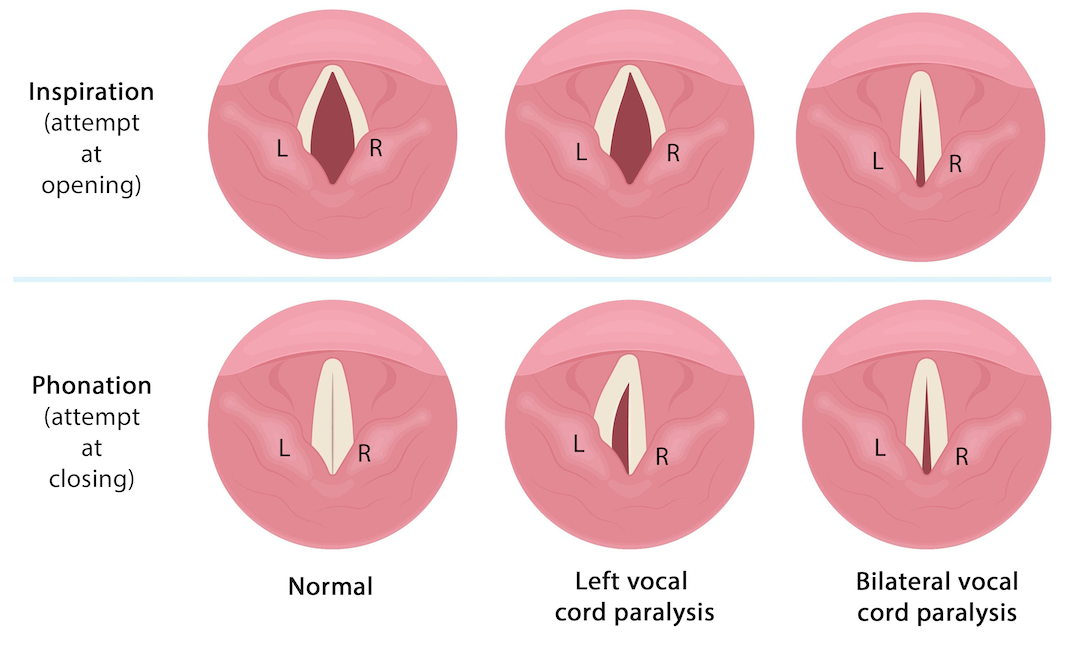
The images on the left are views of the vocal cords from above.
The recurrent laryngeal nerves activate the muscles that move the vocal cords open and closed. Normally, the vocal cords open widely for maximal airflow, such as during an inspiration. And normally, the vocal cords close during swallowing (to keep food and liquid from going down to the lungs) and while making a voice (so that the vocal cords can vibrate against each other, generating a strong sound). The right recurrent laryngeal nerve moves the right vocal cord and the left recurrent laryngeal nerve moves the left vocal cord. The vocal cords are attached together in a fixed position in the front, and the back sides move outwards to open them, making the shape of a triangle.
The external branch of the superior laryngeal nerve on each side activates the cricothyroid muscle. When activated, this muscle lengthens the vocal cords so that a higher pitch of voice may be achieved.
The internal branch of the superior laryngeal nerve on each side provides sensation to the larynx.
What is vocal cord weakness or paralysis?
Since the recurrent laryngeal nerve controls the vast majority of muscles accounting for vocal cord movement, dysfunction of this nerve causes more significant symptoms than for the superior laryngeal nerve. Complete immobility of a vocal cord is termed paralysis, whereas partial immobility is called weakness (or paresis). If both vocal cords are affected, this is bilateral, whereas when one is affected, it is termed unilateral. The degree of symptoms generally correspond to the degree of immobility, and a slight weakness may be of minimal detriment to function. Essentially, the smaller the aperture achievable during respiration increases resistance to airflow, limiting airflow or requiring increased breathing effort, and possibly causing noisy breathing due to turbulent airflow. While speaking (phonation), weakness of one or both vocal cords limits their ability to contact each other tightly to produce a strong voice. The resulting gap between the vocal cords lets more air escape past the vocal cords than normal during phonation, leading to a breathy sounding voice. Also, since the vocal cords normally close tightly during swallowing to help close off the passageway to the lungs, a gap between the vocal cords may contribute to allowing food or liquid to go into the trachea or lungs instead of the esophagus.
One-sided (unilateral) vocal cord paralysis
When a vocal cord is paralyzed, it usually remains fixed in a semi-closed position. Keep in mind that the vocal cords open widely during inspiration (breathing in) and close during phonation (using one’s voice). One-sided vocal cord paralysis narrows the size of the airway somewhat, but typically not enough to cause an individual to be unable to breathe adequately during most activities. A unilateral vocal cord paralysis will usually fail to allow both vocal cords to make good contact against each other for creating a strong voice, unless the position of the affected vocal cord is surgically changed or the opposite vocal cord compensates by moving past midline to create a small gap between the vocal cords .
Vocal cord paralysis of both vocal cords (bilateral)
Fortunately much less common than unilateral vocal cord paralysis, bilateral vocal cord paralysis causes more severe narrowing of the airway and still not enough tight contact between the vocal cords for making a strong voice.
The airway in someone with bilateral vocal cord paralysis may be adequate during periods of rest, but increased demand for airflow to the lungs during periods of exertion may be unmet. A lessening of the already narrow space between the vocal cords (from swelling, for example), could block the airway completely, causing need for an alternative airway, such as tracheotomy.
In views of the vocal cords from above, the differences between normal opening and closing versus left vocal cord paralysis versus bilateral vocal cord paralysis is shown.
Why are the laryngeal nerves affected by surgery?
The recurrent laryngeal nerves are somewhat variable in location, small, and are located directly in the dissection plane between the thyroid gland, the trachea, and the esophagus during certain operations, including those of the thyroid, parathyroid, upper chest, throat or upper esophagus. Some thyroid glands are adherent to the surrounding tissues due to inflammation or tumor growth. The superior laryngeal nerves are also somewhat variable in anatomy and pass between the thyroid gland and the cricothyroid muscle in the plane of dissection during thyroid surgery. Bleeding can obscure visualization of the anatomy. Prior surgery in the area can significantly alter the anatomy, tissue planes, and the ability to visualize the nerves. Surgery on the left puts only the left laryngeal nerves at risk, and similarly surgery only on the right puts only the right laryngeal nerves at risk. Surgical injury to both left and right laryngeal nerves is rare and would not be possible unless both sides were operated.
It is worth noting that the laryngeal nerves may be affected by conditions other than surgery, such as tumors in the brain or neck, stroke (cerebrovascular accident), viruses, trauma, or neurologic conditions.
What are the symptoms of laryngeal nerve weakness or paralysis?
When one or both vocal cords has restricted movement, voice and airway may be affected. Weakness or full paralysis of one recurrent laryngeal nerve causes a hoarseness that may be characterized as breathy and weak. Weakness or paralysis of one or both external branches of the superior laryngeal nerves creates a lower pitched voice and inability to reach a high pitch. Dysfunction of the internal branch of the superior laryngeal nerve can cause altered sensation of the vocal cords, which may lead to inappropriate “throat clearing” or the opposite, not “clearing the throat” when needed. Weakness or paralysis of both recurrent laryngeal nerves can cause difficulty breathing because the vocal cords are unable to open widely for unrestricted airflow. Bilateral vocal cord paralysis may be an emergency if airflow is severely restricted.
It is important to note that all patients who undergo thyroid surgery can be found to have some change in their voice if we look closely enough. That is, even when a patient or those around the patient cannot identify any change in the patient’s voice after surgery, high sensitivity testing does show some alteration in all patients. Fortunately, the likelihood of severe injury is lower than mild or unnoticeable injury.
How much will laryngeal nerve dysfunction bother someone?
The bother of laryngeal nerve injury is variable, depending on the specific nerve(s) involved, the degree of involvement, and how an individual interprets the changes. The great majority of laryngeal nerve dysfunction causes minimal alteration in a person’s voice. Of those with a more noticeable change, time for healing and compensation, as well as voice therapy exercises often restore the voice. More significant hoarseness may be treated surgically (see below). Altered sensation of the larynx may affect swallowing, though problems are usually evident only when other pre-existing factors predispose or contribute to swallowing dysfunction. Speech and swallowing therapy can often help improve swallowing in this situation.
Does laryngeal nerve injury improve over time?
Often, injury to a laryngeal nerve will improve. This may be due to natural repair and regeneration of the nerve itself, or it may be that (for one sided recurrent laryngeal nerve injury) the opposite vocal cord adapts and compensates, to improve the closure between the vocal cords when appropriate.
How is laryngeal nerve weakness treated?
An emergency related to inadequate airflow between the vocal cords may require intervention, including possible tracheostomy tube placement to create an airway to and from the lungs that bypasses the narrowing between the vocal cords. This is rare and involves a situation in which both left and right recurrent laryngeal nerves are not functioning. The less rare but still uncommon situation of one laryngeal nerve being weak is typically evaluated for any imminent danger, such as difficulty swallowing safely. Speech and swallowing therapy often helps significantly in this scenario. Temporary movement of the affected vocal cord toward midline may be undertaken with a procedure involving injection of a slowly absorbable substance into the vocal cord, which may help the problem temporarily while healing progresses. Once safe laryngeal function has been established, time and therapy are typically utilized. If about a year since one-sided recurrent laryngeal injury passes without adequate return of function, a procedure involving moving the affected vocal cord toward midline in a more permanent fashion may be undertaken. For patient with bilateral vocal cord paralysis and a tracheostomy, the tracheostomy tube can often be safely removed if vocal cord movement returns or if a procedure to create a greater opening between the vocal cords is undertaken.