Conditions: Thyroid Nodule
Thyroid nodules are growths or lumps that form within the thyroid gland. A thyroid nodule may be hyperactive, producing too much thyroid hormone. A thyroid nodule might also grow large enough to compress nearby structures, causing difficulties. And since about 5% of all nodules are cancerous, evaluation of a thyroid nodule is undertaken to determine what, if any, treatment is necessary.
Thyroid gland
About the thyroid gland
The thyroid gland produces thyroid hormone, which is an essential driver of metabolism and many organ functions. Without adequate thyroid hormone, either due to the gland dwindling production due to disease or from surgery or radiation, a hypothyroid state develops in which an affected individual may begin to become fatigued, gain weight, tolerate cold temperatures poorly, and experience a poor cognitive function and depression. Too much thyroid hormone, either from an overactive thyroid gland (or part of it), or an excess of thyroid hormone replacement medication leads to symptoms of anxiety, jitteriness, tremor, a faster and even irregular heart rate, as well as bone density loss. Thyroid hormone itself contains iodine, which must come from our diet, and the thyroid is the only organ that uses iodine. The thyroid gland is located in the low neck, draped across the windpipe just above the sternum.
thyroid nodule
The word nodule simply means a lump or area different from its surroundings. A given individual may have no nodules, one nodule, or more than one nodule. Thyroid nodules are very common, yet only 5% of thyroid nodules are cancerous. Non-cancerous nodules may be of no importance or sometimes they produce excess thyroid hormone or even get so big as to compress nearby structures. Once a thyroid nodule is identified, blood testing and an ultrasound are typically performed.
Thyroid nodules are typically painless, but can be painful in some situations.
Hyperfunctioning thyroid nodule
A hyperfunctioning thyroid nodule, also known as a toxic adenoma, is a common condition characterized by the abnormal growth of some thyroid tissue (the nodule) that produces excess thyroid hormone. Not every thyroid nodule produces excess thyroid hormone, but when one does, it fails to decrease production of thyroid hormone when it should because it does not respond appropriately to feedback system whereby the pituitary gland reduces its production of thyroid stimulating hormone. Instead, the hyperfunctioning nodule inappropriately secretes excess thyroid hormone which leads to hyperthyroidism. A hyperfunctioning nodule is rarely malignant. The location of a toxic adenoma may be identified with a radioiodine uptake scan.
Nonfunctioning nodules
Thyroid nodules that do not thyroid hormone are called nonfunctioning nodules. These are common in the population and may exist as a single nodule or among several nodules in a given thyroid gland. In general, about 5% of all nonfunctioning nodules are cancerous, and therefore do not require surgery unless their size becomes problematic.
Thyroid cancer
The word cancer means a growth that has potential to invade surrounding tissues aggressively and spread to other parts of the body, and is therefore more dangerous than a benign tumor that does not spread like that.
Once a thyroid nodule is discovered, how is it evaluated?
Since a thyroid nodule is commonly identified by physical exam or incidentally by an imaging technique (like CT or MRI) undertaken for another purpose, a thyroid ultrasound and a blood draw testing for hypothyroidism and hyperthyroidism is typically undertaken.
ultrasound
There are many ways thyroid abnormalities may be detected, but the cornerstone method to evaluate them is with an ultrasound (sonogram). Using only sound waves, an ultrasound not only provides generally more useful information for thyroid nodules than other types of imaging, but it also avoids radiation exposure or need for an I.V., and does not involve a magnet or the patient being positioned in a small tunnel as with CT or MRI. Information from a thyroid ultrasound allows each nodule to be assigned a numerical risk score. Called the “TI-RADS” scoring, this system provides a standardized way to assess the danger of a given nodule and to guide how management should proceed. Some nodules demonstrate ultrasound features that reliably indicate that they are benign, and so no further testing or intervention would be necessary for that nodule. Nodules scored to have low to intermediate risk are followed with a repeat ultrasound after a year. Nodules that appear on ultrasound to have higher risk of being cancerous malignancy are identified for needing a needle biopsy to further investigate for cancerous cells. Needle biopsies are usually done simultaneously with an ultrasound to verify accuracy of needle placement.
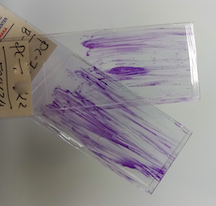
Needle biopsy
Typically, a thyroid ultrasound provides information to determine if a needle biopsy is needed, as noted above. A fine (thin) needle biopsy is a safe way to obtain some tissue from a given nodule and assess it in the laboratory. A needle biopsy (specifically, a fine needle aspiration, or FNA) is typically performed with simultaneous use of an ultrasound to assist with the precise anatomic positioning of the needle to obtain cells from the nodule of concern. In this procedure very small sampling of cells is obtained. While the technique and needle movements of a fine needle biopsy differ from how a blood draw or I.V. placement is performed, the risk is essentially the same, which is a major advantage of this technique. Some discomfort and possible bruising may occur. While no one likes needles, the risk of a needle biopsy is very low and the information gained is valuable. A needle biopsy result usually indicates whether surgery is needed. The Bethesda system is a well-established classification scheme for reporting thyroid fine needle aspiration results and serves as a basis for recommended actions.
Genetic testing of a thyroid nodule
Examination under a microscope of the cells obtained from a needle biopsy may provide adequate information to know, with reasonable certainty, whether a nodule is cancerous or benign. When this is the case, thyroid surgery may be recommended. But what is to be done with thyroid nodules that are not clearly benign and not clearly cancerous despite use of ultrasound and sampling of the cells with a fine needle aspiration biopsy? This dilemma is especially common when the fine needle aspiration result is reported to be a follicular lesion because one specific type of thyroid cancer called follicular carcinoma cannot be differentiated from a benign follicular adenoma on the basis of needle biopsy.
Traditionally, a nodule that is suspicious but indeterminate for cancer even after the techniques described above could be either observed with repeat ultrasound and possibly repeat biopsy after about a year or thyroid surgery could be undertaken for a definitive answer.
Recently, the use of genetic testing on the sample obtained from a thyroid nodule fine needle aspirate has been promoted as a better way to assess risk of cancer for an indeterminate risk nodule. This has great appeal to many since the testing for certain genetic mutations in the needle biopsy sample could, in theory, determine whether a nodule is cancerous and therefore needs surgery versus a benign nodule for which surgery could be safely avoided.
While the need for a definitive non-surgical method to assess for cancer in a thyroid nodule has long been recognized, the promise of genetic testing for this purpose has not been fully realized. Multiple companies have developed genetic testing of the specimen to look for markers of cancer, and while the science is slowly improving, at present no genetic marker can definitely rule in or rule out malignancy for these suspicious but indeterminate nodules. Currently, these tests can usually increase or decrease the apparent likelihood that a given nodule is cancerous, but often not significantly. For example, if risk for cancer in a nodule is thought to be 25% using non-genetic testing, when genetic testing changes this risk to either 15% or to 45%, the decision-making for surgery may not be meaningfully changed. Typically, the patient has a significant out-of-pocket cost for these tests and if no surgery is performed, the thyroid nodule likely still needs further monitoring by a physician. The first four commercial tests available are Afirma gene expression classifier (Afirma-GEC), ThyGenX/ThyraMIR, ThyroSeq, and RosettaGX Reveal.
HOW TO GET THE MOST FROM YOUR APPOINTMENT
Appointment time is valuable. Below are some suggestions to make the most of your appointment. This preparation will help you and your doctor maximize efficiency and accuracy, freeing up time for questions and answers.
This page