Conditions of Balance
Few experiences are as memorably unpleasant as episodes of dizziness. Sensing our position with respect to gravity and our surroundings is based on input to the brain from several different systems. An aberrancy of one or more of these systems can create a sense of imbalance. Identifying the cause of imbalance is the key first step toward restoration of normalcy.
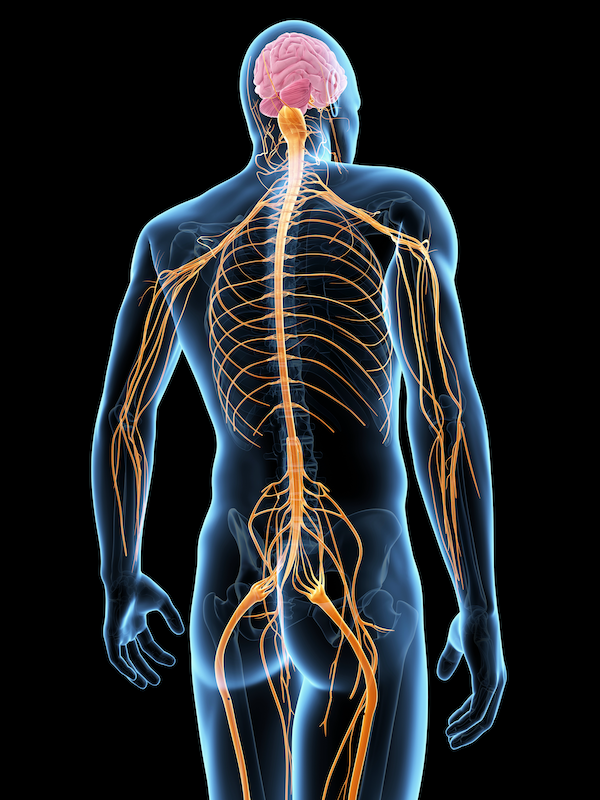
The balance system
Balance is our perception of our position in space. Our sense of balance comes from three main systems (vestibular or inner ear, visual, and proprioception), each providing information to a part of the brain called the cerebellum. When the inputs from various systems contradict each other, a very unpleasant sensation arises which goes by various names but could be called disequilibrium or imbalance. Vertigo is one specific type of imbalance in which a spinning or rotational sensation predominates.
• Animated video explaining function of the inner ear vestibular system.
BPPV (Benign paroxysmal positional vertigo)
Benign paroxysmal positional vertigo (BPPV) is a common disorder arising from a problem in the inner ear causing repeated, brief periods of vertigo (dizziness feeling like spinning or rotation). A given vertigo event from BPPV occurs with changes in the position of the head, such as rolling over in bed, starts suddenly, and typically lasts less than one minute, but often causes nausea.
BPPV occurs as a result of displacement of calcium crystals known as otoconia or otoliths from their normal position, most likely those in the otolithic membrane of the utricle. After their displacement, they typically settle in the posterior canal, thus rendering it sensitive to gravity when it would normally be sensitive to rotation. Variants of posterior canal BPPV exist, such as when otoconia float freely in one of the horizontal or superior semicircular canals (horizontal or superior) or in the cupula. Diagnosis of BPPV is made by history, physical exam, and use of the Dix-Hallpike diagnostic maneuver. Treatment involves moving the displaced otoconia back to their normal position, typically done with the Epley maneuver. and typically performed by an audiologist or physical therapist.
Meniere’s disease
Ménière's disease is a disorder of the inner ear that is characterized by episodes of feeling like the world is spinning (vertigo), ringing in the ears (tinnitus), hearing loss (usually in the low frequencies), and a fullness in the ear. Typically, only one ear is affected initially; however, over time both ears may become involved. Episodes generally last from 20 minutes to a few hours, and a variable length of time may pass between episodes. Hearing loss and ringing may at first be present only during attacks, but over time can become constant.
Diagnosis is based on the symptoms and, frequently, a hearing test. Other conditions that may produce similar symptoms include vestibular migraine and transient ischemic attack.
vestibular migraine
Vestibular migraine is vertigo associated with a migraine, either as a symptom of migraine or as a related distinct neurological disorder. Diagnostic criteria for vestibular migraine by the International Headache Society are:
A. At least 5 episodes with vestibular symptoms of moderate or severe intensity, lasting 5 minutes to 72 hours
B. Current or previous history of migraine with or without aura according to the International Classification of Headache Disorders (ICHD)
C. One or more the following migraine features associated with at least 50% of the vestibular episodes:
- headache with at least two of the following characteristics: one sided location, pulsating quality, moderate or severe pain intensity, aggravation by routine physical activity
- photophobia (aversion to bright lights) and phonophobia (aversion to loud sounds)
- visual aura
D. Not better accounted for by another vestibular or ICHD diagnosis
heart and vascular causes for dizziness
Of the many causes of dizziness, blood flow to the brain is a relatively common one. Low blood pressure even temporarily due to dehyration, standing up quickly, medicine to reduce blood pressure, or an irregular heart rhythm are some specific potential causes of dizziness from low brain blood flow. These conditions are managed by a cardiologist.
Neurologic causes for dizziness
Dizziness caused by brain conditions (such as stroke, multiple sclerosis, brain tumor) are managed by a neurologist, and appropriate referral can be made. Initiating physical therapy to help with imbalance and compensation is sometimes begun as the neurology referral is made.
Mal de debarquement syndrome
Mal de debarquement syndrome (or disembarkment syndrome) is a neurological condition usually occurring after a cruise, aircraft flight, or other sustained motion event. The phrase "mal de débarquement" is French and translates to "illness of disembarkment. Typical symptoms include a persistent rocking, swaying, or bobbing feeling (despite the absence of ongoing motion). Because most vestibular testing proves to be negative, doctors may be baffled as they attempt to diagnose the syndrome. A major diagnostic indicator is that most patients feel better while driving or riding in a car, i.e, while in passive motion. Mal de debarquement syndrome is unexplained by structural brain or inner ear pathology and most often corresponds with a motion trigger, although it can occur spontaneously. This differs from the very common condition of "land sickness" that most people feel for a short time after a motion event such as a boat cruise, aircraft ride, or even a treadmill routine which may only last minutes to a few hours. Diagnosis is clinicial—the history may be supportive but there are no definitive tests to confirm mal de debarquement syndrome, although tests ruling out other conditions may be indicated.
Proprioception and dizziness
One’s perception of their movement and position in space depends heavily on feedback from muscles and joints from the legs up to the neck. Hip and knee replacements as well as arthritis or other changes in the spine can result in proprioceptive changes that do not correspond to what the eyes and ears are telling the brain. The discordance of information leads to dizziness.
how to get the most from your balance appointment
Appointment time is valuable. Here are some suggestions to make the most of your appointment. This preparation will help you and your doctor maximize efficiency and accuracy, freeing up time for questions and answers.
This page